 Last week the trustees of the Medicare program, whose 50th anniversary is this Thursday (see accuracy.org/calendar), released their annual report. It showed that traditional Medicare overhead amounts are about 2 percent of the program’s expenditures. That figure sharply contrasts with the 12 percent to 14 percent overhead typical of private health insurance companies. [PDF]
Last week the trustees of the Medicare program, whose 50th anniversary is this Thursday (see accuracy.org/calendar), released their annual report. It showed that traditional Medicare overhead amounts are about 2 percent of the program’s expenditures. That figure sharply contrasts with the 12 percent to 14 percent overhead typical of private health insurance companies. [PDF]
A recent study published at the Health Affairs Blog shows that the private insurance-based Affordable Care Act — sometimes called “Obamacare” — will add more than a quarter of a trillion dollars to the already very high administrative costs of U.S. health care through 2022. Nearly two-thirds of this new overhead — $172.2 billion — will go for increased private insurers’ administrative costs and profits.
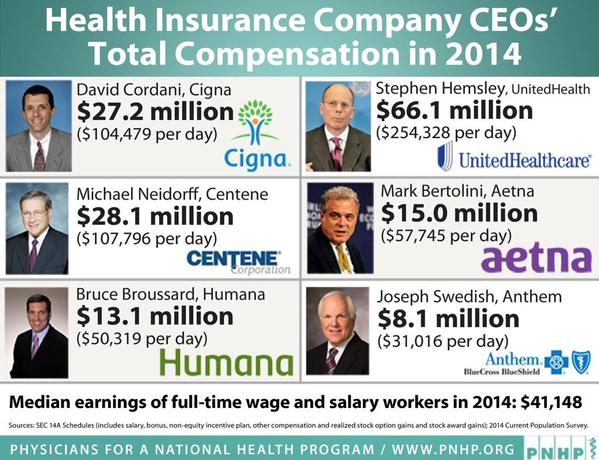
AP reports in “Why the 2010 Health Care Law Led to Insurance Merger Mania“: “The health care overhaul law has reshaped the health insurance business, and one consequence is more than $100 billion in mergers and acquisitions over the last few years. Anthem Inc.’s purchase of Cigna Corp. and Aetna Inc.’s acquisition of Humana Inc., both announced this month, are worth more than $80 billion combined. … Many of [these] purchases have been designed to bulk up their [private] Medicaid and Medicare Advantage businesses because both of those programs keep growing.”
Interviews are available with the following:
STEFFIE WOOLHANDLER, M.D., swoolhan at hunter.cuny.edu
DAVID HIMMELSTEIN, M.D., dhimmels at hunter.cuny.edu
MARK ALMBERG, mark at pnhp.org, @pnhp
Woolhandler and Himmelstein are co-authors of the recent Health Affairs Blog study titled “The Post-Launch Problem: The Affordable Care Act’s Persistently High Administrative Costs.” They are professors at the City University of New York’s School of Public Health, longtime researchers in U.S. health care, and co-founders of Physicians for a National Health Program, an organization that advocates for a single-payer health care system. Almberg is communications director at PNHP and can facilitate interviews with Woolhandler and Himmelstein.
In a recent interview, Himmelstein said that the latest merger plans, if approved by regulators, “will leave us with a small handful of insurance giants that are essentially monopolies. Much of their revenue comes from the government that pays hundreds of billions annually in premiums for private ‘Medicare Advantage’ plans, Medicaid managed care plans, and much of the premiums for the private plans bought on [ACA] insurance exchanges. Much of this money is wasted; Anthem and Cigna have overhead that’s nearly tenfold higher than traditional Medicare.”
What’s more, Himmelstein continued, “These monopolies are lightly regulated, and have used their enormous financial and political clout to avoid real oversight. Just this month, the insurers’ lobbying group hired as their new CEO Marilyn Tavenner, who as head of Medicare and Medicaid was responsible for regulating them until this spring.”
Woohandler said today: “Between 2014 and 2022, the ACA will add $273.6 billion in new administrative costs over and above what would have been expected had the law not been enacted. That’s equivalent to $1,375 per newly insured person per year, or 22.5 percent of total federal expenditures for the program.”
She added: “Were the 22.5 percent overhead figure associated with the ACA to drop to traditional Medicare’s level, the U.S. would save $249.3 billion by 2022. In health care, public insurance gives much more bang for each buck.”